November 29, 2022
Note: This resource is intended to be useful both as a standalone document, as well as the fourth part of Business Group on Health’s Value-Based Purchasing Guide. Click the link to access additional parts related to other elements of employer value-based purchasing strategy.
Accountable care organizations (ACOs) and high-performance networks (HPNs) are groups of providers selected based on their quality credentials that can provide comprehensive care and accept performance risk for an entire population within a geography. Other common value-based arrangements, like centers of excellence (COEs) or direct primary care (DPC), focus on a smaller population of plan members or a subset of patient care.
There are parallels in the uptake of ACOs and HPNs, as they have emerged as two of the primary ways to introduce value-based purchasing for a broad pool of patients. In the Business Group’s own annual large employer member survey, 30% of respondents said they make ACOs available to their employees and 43% said the same regarding HPNs in 2023.
What Are ACOs and HPNs?
An ACO is a group of providers, such as hospitals, primary care physicians, specialists and other health care professionals, who agree to take on financial responsibility for the cost, health outcomes and consumer experience of care for a defined population. ACOs are groups of providers that operate collectively under a value-based arrangements. ACOs manage which providers are included in their network, and coordinate care and proactively reach out to patients in partnership with them. An ACO can be a sole network for a health plan in a designated geography, or it can be embedded in a traditional PPO plan that allows patients to select ACO or non-ACO providers.
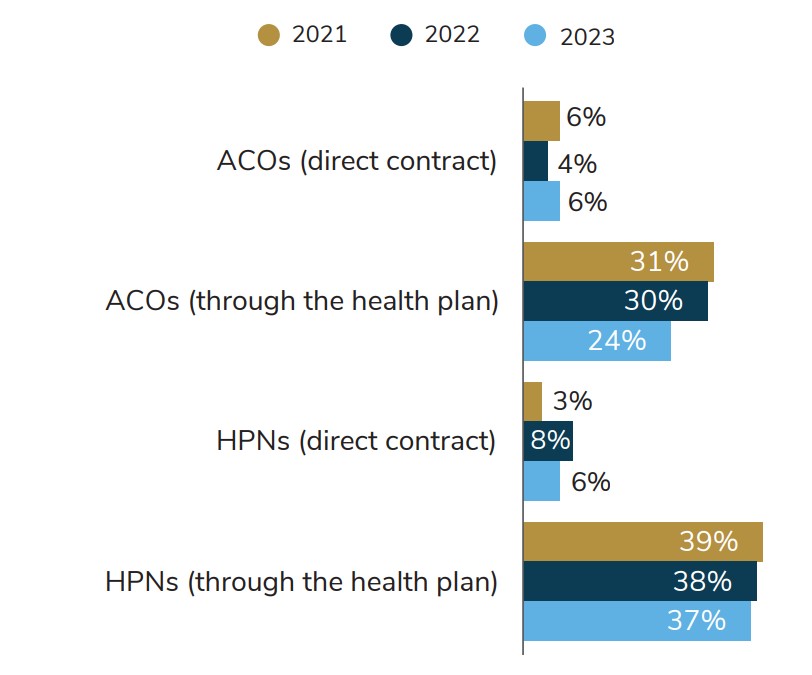
Source:2023 Large Employers’ Health Care Strategy and Plan Design Survey
HPNs, on the other hand, are network configurations that limit provider participation to only those who have met certain high standards for quality of care at a lower cost. Unlike an ACO, providers in an HPN do not necessarily work in a coordinated system or take financial risk for their outcomes, but they will only stay in-network and have access to patients who have selected the HPN if they maintain their high-quality scores and lower costs. HPNs often include multiple ACO providers in their networks, but the value-based arrangements with those ACOs are generally managed by a health plan curating the HPN, instead of directly by the employer.
How Prevalent Are ACOs and HPNs?
HPNs are offered in most major regions in the U.S. through all major health plans. There is also a growing sector of third-party vendors that employers can contract with to organize HPNs outside of traditional health plan negotiations. Using a vendor gives employers more flexibility over how they select those networks but requires building an additional vendor relationship.
ACOs are also widespread in the U.S., with the Centers for Medicare and Medicaid Services contracting with 483 of them alone in 2022.13 ACOs may take on ACO contracts with multiple payers, including both public and commercial. ACOs are concentrated in urban centers where there are more patients and providers. In the U.S., 42.7% of doctors participate in a commercial ACO in 2020, up from 31.7% in 2016.14 This prevalence of ACOs/HPNs and growing participation by providers creates a significant opportunity for employers to influence the delivery system through ACO/HPN contracting.
How Are ACOs and HPNs Reimbursed?
Reimbursement structures for ACOs run the full spectrum of population-based approaches laid out in Part 2: Value-Based Reimbursement Strategies. These include shared savings, shared risk and capitation. Individual services, such as surgery, provided by the ACO may also be paid for in a bundled payment structure.
Most ACOs in the Medicare Shared Savings Program only operate in shared-savings arrangements, while 37% accept some form of shared risk.15 Many provider groups are unwilling to accept financial risk in contracting because they don’t have the cash reserves to pay penalties if they have a bad year or are not confident in their ability to achieve financial targets.16 Reimbursement for ACOs in health plan contracts is less standardized than in Medicare, but they are paid more often in shared-savings rather than shared-risk arrangements.
HPN participating providers are generally reimbursed through fee-for-service (FFS), but must maintain high quality scores to remain eligible to accept patients who selected an HPN.
Why Would an Employer Contract with an HPN and/or an ACO?
There are advantages and disadvantages to implementing an ACO or HPN strategy, though they are not mutually exclusive. They are both geographically focused strategies, which means that an employer may offer ACO plans in some regions and HPNs in others. In a given geography, both ACOs and HPNs could be offered as plan options.
ACOs are run by physician groups, integrated health systems or hospital and physician partnerships that contract directly with payers. There are three predominant ways that ACOs are organized:
- By single health systems that include the full spectrum of care a patient might need.
- By a consortium of provider groups and hospitals that come together to form an ACO that collectively shares responsibility for the care of the patients assigned, or attributed, to them.
- Through primary care groups that do not have hospitals in their ACO ownership; the ACO is still responsible for the total cost of care for the population attributed to them, but the primary care groups decide where to refer patients for specialty and hospital care outside of their ACO providers in a broader PPO-like network.
Table 4.1 describes key characteristics of each approach, pointing out key differences.
Table 4.1: Characteristics of HPNs and ACOs
| Characteristic | High-performance Networks | Accountable Care Organizations |
|---|---|---|
| Geography | Can be set up in multiple regions, potentially attractive for multistate employers | Limited to a single region where the ACO providers operate |
| Payment Models | FFS with elements of risk sharing, but providers must maintain high quality and lower costs to participate as defined by network participation criteria | Shared savings, shared risk and capitation reimbursements are the most common value-based payments |
| Clinical Model | Providers are not necessarily connected to each other | Providers organize themselves and coordinate care, often through existing health systems, though significant variation in level of execution exists |
| Insurance Model | Offered as a standalone insurance option during open enrollment or embedded within a broader PPO network with steerage to encourage use of HPN providers | Can be offered as a standalone insurance option, but more often than not is organized by health plans and embedded into a PPO network |
| Contracting | Through a health plan or direct contract | Through a health plan, direct contract or third-party vendor |
| Network Size | In-network providers will be fewer than in a standard PPO because there are higher quality and cost efficiency requirements for participation | Varies based on the size of the ACO, but it is generally smaller than a standard PPO network |
How Do ACOs and HPNs Fit Into Employer Benefits Strategy?
Most employers select ACO and HPN partners that have been contracted by their health plans. A smaller portion of large employers contract directly with ACOs and HPNs in locations where they have a large employee base. Direct contracting gives employers greater influence on contracted quality and budgetary metrics. However, it requires additional resources and expertise within a benefits team to direct and manage those relationships, as well as a significant enough employee base to make such a relationship viable for a provider group.
If those requirements can be met, there are many reasons why an employer can benefit from contracting with an ACO or HPN.
Opportunities to Transfer Traditional Benefits Tasks to ACO Providers
As risk-bearing entities with clinical expertise, ACOs can be an ideal delivery method for services that have traditionally been carried out by health plans, such as care coordination, proactive outreach to plan members about recommended screenings and health benefit programs offered by the employer. Given that ACOs can take on some of the roles that health plans and other point solutions (e.g., a diabetes management provider) traditionally manage, employers should consider where some of these functions can be “turned off” for plan members attributed to an ACO because the ACO itself will take them on.
As networks of high-performing but not necessarily clinically integrated providers, HPNs are less equipped to take on some of these responsibilities from health plans or employers. On the other hand, this also means that employers don’t need to rethink their care coordination, employee outreach or other strategies in a market with an HPN in the way that they might with an ACO partnership.
Interaction Between Other Provider Groups Employers Contract With
Large employers regularly contract with on-site clinics (53% of employers in 2023) and Centers of Excellence (COEs) (90% of employers with at least one in 2023.) Many employers have value-based reimbursement arrangements with these providers and will need to address with their provider partners who is financially responsible for the care of a patient who is, for example, attributed to a ACO but gets treatment from a COE provider for a particular procedure. ACOs may want to keep plan members within their networks for procedures that an employer has contracted with another COE provider to do. Member communication will need to be streamlined so as not to confuse patients.
Impact on Integrated Benefits Offerings
Employers introducing ACOs or HPNs into their benefits strategy need to consider how these arrangements not only affect other network strategies they may deploy, but also other vendor relationships they may have that touch patients attributed to the ACO or HPN. For example, should an employee in an ACO or HPN that provides enhanced clinical condition management programs still be offered third-party vendor programs at the employer’s expense if the programs could end up being duplicative? How do you decide which program or value-based provider group improved outcomes if both impacted the patient? There isn’t necessarily one correct answer, but employers will need to answer these questions for themselves.
Once again, an HPN won’t necessarily require the same considerations as listed above for ACOs. However, a patient in an HPN getting a referral from their primary care provider may need additional navigation to make sure they do not go outside their network.
Local Market Dynamics
The location of an employer’s workforce and the health care delivery system dynamics of a given market will have an outsized impact on what ACO or HPN strategy may be best for an employer.
Workforce considerations by market include:
- The number of employees and family members who live in a given region, including those working remotely. ACOs are likely more appropriate for concentrated populations, whereas HPNs are viable even for disbursed employee populations through health plan arrangements.
- Where employees work and live within a market compared to health system assets. As virtual care proliferates, this is less of a concern, but in some large metro areas, the location of an ACO or HPN hospital, for example, might be an hour- long drive across town, even if they are in the same city. Employers need to do an assessment of where their work locations and employees’ homes are compared to ACO or HPN providers, keeping in mind that the white collar workforce increasingly works from home and not in centralized offices.
- Workforce health and historical spending patterns. In markets where an employee population is already relatively healthy or has low health care costs, employers may want to avoid disruption associated with implementing an ACO or HPN strategy.
- Other large employers in the market willing to partner to increase bargaining power and have an employee pool sizeable enough for a direct contract. There are some markets where large employers are working together to create direct contracts with health care providers taking on ACO contracts.
Delivery system considerations by market include:
- The level of competition between health care systems and primary care groups. If a region’s delivery system is overly consolidated, it may be difficult to find provider partners that are meaningfully better performing than the market of competing providers in the region. Consolidated markets have provider systems – particularly those with hospitals – with outsized bargaining power, which means that a value-based primary care focused strategy may be best; PCPs with appropriate technology and data can help patients navigate to high- quality providers within hospital systems without an employer needing to contract separately for hospital services.
- The prevalence of out-of-network care delivery in a given market. An ACO or HPN strategy in a market with high out-of-network care may be attractive because the ACO has a greater incentive to keep patients in the ACO network and the HPN has high- quality doctors available to patients when they need them.
- The historical performance of an ACO or HPN in that market. There is variation of value-based performance by ACOs and HPNs within and across markets. ACOs began to take shape in the ‘00s and were accelerated by the passage of the Affordable Care Act in 2010, which means that many have more than a decade of performance data to review before making the decision to implement an ACO strategy. For HPNs, there are performance cutoffs for providers to participate in the network, which means that health plans and third-party organizers of HPNs should be able to easily share past quality and cost performance of HPNs.
Conclusion
An employer’s ability to drive improvements in health care quality, employee health outcomes and health care spending through an ACO or HPN partnership will depend on many factors both within and out of their control based on the markets they’re considering. Employers should look for strong provider and health plan partners who are transforming the way care is delivered and seek to drive employees to those high-performing provider groups.
Population health approaches like these can take years to make significant improvements in health outcomes. There are some quality metrics, like screening and vaccination rates, and some patient experience measures where you can improve provider metrics within a plan year. But for health care outcomes like blood pressure control, A1c control or readmission reductions, there are often significant changes that providers and patients need to make to address and improve them. This is a multiyear journey, but often a worthwhile one for employers.
Employer Recommendations
- 1 | Identify markets where you have a significant employee presence, then look to the local dynamics of that geography to determine whether an ACO strategy is appropriate for that market. Direct contracting will likely require 1,000 or more employees and dependents in the geography for providers to be interested.
- 2 | In geographies where an ACO strategy isn’t viable, consider implementing an HPN through your health plan or third-party vendor. This strategy does not require as many employees in a geography because health plans and other vendors can aggregate populations across several employer clients.
- 3 | Ask your health plan partners for data on their ACO and HPN performance in your markets of interest. ACOs and HPNs are not standardized across markets given that health care is local, so an ACO/HPN may be attractive in some but not all your markets. If you pursue a value-based contract with an ACO or HPN directly or through a third party, make sure to regularly monitor performance on these metrics over time. Continuous quality improvement should be an expectation, especially if you are using plan design levers to encourage plan members to go to participating providers.
- 4 | Consider which key elements of an ACO contract may be necessary to have in place for you to feel comfortable moving forward. This includes many aspects covered in other parts of the Value-Based Purchasing Guide, such as quality metrics you’re interested in holding providers accountable for, virtual care capabilities, ability to integrate with other elements of your benefits strategy, and the payment models you need to have in place to feel confident about your ACO strategy.
- 5 | Decide whether it is more appropriate to offer a standalone insurance option for ACOs/HPNs that have comprehensive networks that will cover a patient’s full set of health care or, instead, provide incentives for plan members to get care from ACO/HPN providers within a broader PPO network. A standalone insurance option will steer more coverage to participating providers, which may net employers better contract terms because the benefit to providers is greater. On the other hand, engagement strategies (e.g., communications, plan design incentives, etc.) to encourage plan members to go to ACO/HPN providers within a broader PPO will be easier to administer and doesn’t require a significant employee base in a particular geography.
- 6 | Consider which elements of benefits administration may be able to be carved out for those employees in high-performing ACOs. This could include benefits like employee navigation services, care management and utilization management. This type of arrangement requires coordination with health plans and other vendors that are delivering these services to your broader population. It may be advantageous for a plan member’s provider team to carry out some of these services given their ability to connect the administrative and clinical capabilities that third parties cannot.
More Topics
Articles & Guides- 1 | Centers for Medicare & Medicaid Services. Performance Year 2021 APM Performance Pathway: CMS Web Interface Measure Benchmarks for ACOs. Quality Payment Program. Accessed October 11, 2022. https://qpp-cm-prod-content.s3.amazonaws.com/uploads/1306/Performance%20Year%202021%20APM%20Performance%20Pathway-CMS%20Web%20Interface%20Measure%20Benchmarks%20for%20ACOs.pdf
- 2 | The Leapfrog Group. Preventing and Responding to Patient Harm. Leapfrog Ratings. Accessed October 11, 2022. https://ratings.leapfroggroup.org/measure/hospital/preventing-and-responding-patient-harm
- 3 | Agency for Healthcare Research and Quality. About CAHPS. July 2022. Accessed October 11, 2022. https://www.ahrq.gov/cahps/about-cahps/index.html
- 4 | Conti R et al. Projections of US Prescription drug spending and key policy implications. JAMA Health Forum. 2021;2(1). https://jamanetwork.com/journals/jama-health-forum/fullarticle/2776040. Accessed November 8, 2022.
- 5 | Business Group on Health. Emerging Trends in Cancer Care. October 25, 2021. https://www.businessgrouphealth.org/resources/emerging-trends-in-cancer-care. Accessed November 8, 2022.
- 6 | Golden W et al. Changing how we pay for primary care. New England Journal of Medicine Catalyst. November 20, 2017. https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0326. Accessed November 8, 2022.
- 7 | Bitton A et al. Off the hamster wheel? Qualitative evaluation of a payment-linked patient-centered medical home (PCMH) pilot. The Milbank Quarterly. 2012 Sep; 90(3): 484–515. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3479381/. Accessed November 8, 2022.
- 8 | Primary Care for Boeing’s Mesa Employees. Iora Health. Accessed on February 9, 2022. https://ioraprimarycare.com/boeing/
- 9 | Bleser W, et al Half a decade in, Medicare accountable care organizations are generating net savings: Part 1. Health Affairs Blog. September 20, 2018. https://www.healthaffairs.org/do/10.1377/forefront.20180918.957502/full/. Accessed November 8, 2022.
- 10 | Sullivan G, Feore J. Physician-led accountable care organizations outperform hospital-led counterparts. Avalere. October 15, 2019. https://avalere.com/press-releases/physician-led-accountable-care-organizations-outperform-hospital-led-counterparts. Accessed November 8, 2022.
- 11 | Business Group on Health. 2023 Large Employers’ Health Care Strategy and Plan Design Survey. https://www.businessgrouphealth.org/resources/2023-plan-design-health-care-delivery-system. Accessed November 8, 2022.
- 12 | Lapsey H. The Better Benefit Stack. 2018 Oliver Wyman Health Innovation Journal. https://health.oliverwyman.com/2019/03/the-better-benefit-stack.html
- 13 | Centers for Medicare & Medicaid Services. Medicare Shared Savings Program Continues to Grow and Deliver High-Quality, Person-Centered Care Through Accountable Care Organizations. CMS Newsroom. January 26, 2022. https://www.cms.gov/newsroom/press-releases/medicare-shared-savings-program-continues-grow-and-deliver-high-quality-person-centered-care-through. Accessed November 8, 2022.
- 14 | O’Reilly K. Doctor participation in ACOs, medical homes grows amid pandemic. American Medical Association. December 7, 2021. https://www.ama-assn.org/practice-management/payment-delivery-models/doctor-participation-acos-medical-homes-grows-amid. Accessed November 8, 2022.
- 15 | Avalere. MSSP Sees Continued Growth in Downside Risk ACOs. January 21, 2020. https://avalere.com/insights/mssp-sees-continued-growth-in-downside-risk-acos. Accessed November 8, 2022.
- 16 | Mechanic R et al. The 2018 Annual ACO Survey: Examining the Risk Contracting Landscape. Health Affairs Forefront. April 23, 2019. https://wwwhealthaffairs.org/do/10.1377/forefront.20190422.181228/full/. Accessed November 8, 2022.
- 17 | Business Group on Health. 2023 Large Employers’ Health Care Strategy and Plan Design Survey. https://www.businessgrouphealth.org/resources/2023-large-employers-health-care-strategy-and-plan-design-survey
- 18 | Business Group on Health. 2023 Large Employers’ Health Care Strategy and Plan Design Survey. https://www.businessgrouphealth.org/resources/2023-plan-design-health-care-delivery-system.
- 19 |Elkins K. Lowe's free surgery program helps cut costs, benefit employees. Charlotte Business Journal. March 30, 2016. https://www.bizjournals.com/charlotte/blog/outside_the_loop/2016/03/lowe-s-free-surgery-program-helps-slice-costs.html. Accessed November 8, 2022.
-
IntroductionValue-based Purchasing Employer Guide: Introduction
-
Executive SummaryValue-based Purchasing Employer Guide: Executive Summary
-
Part 1Definitions and Measures of Value in Value-based Purchasing
-
Part 2Value-based Reimbursement Strategies
-
Part 3Value-based Primary Care
-
Part 4Accountable Care Organizations and High-Performance Networks
-
Part 5Centers of Excellence
-
Part 6Value-based Virtual Care
-
Part 7Value-based Care Engagement Strategies
This content is for members only. Already a member?
Login
![]()
